A recent study published in the journal PNAS Nexus has revealed the extensive impact of human antibiotic use on global river systems, highlighting the presence of antibiotic pollution at levels that exceed ecological safety thresholds. This contamination poses risks to aquatic ecosystems and raises concerns about the development of antimicrobial resistance (AMR), a major public health challenge worldwide.
Researchers employed an advanced contaminant fate model called HydroFATE to estimate the quantities of 40 commonly used human antibiotics reaching rivers and oceans from domestic sources. Their analysis, spanning 23.8 million kilometres of global river networks, estimated that around 8,500 tonnes of antibiotics enter river systems annually from human use alone.
Global human antibiotic consumption was estimated at approximately 32,200 tonnes per year, with the 40 antibiotics studied accounting for about 30,300 tonnes. Of this total, around 68 per cent (20,500 tonnes) is excreted by people, and close to 29 per cent of that load (8,500 tonnes) enters rivers. The research found that only 43 per cent of antibiotics from domestic wastewater are treated effectively, with centralised treatment plants removing about 72 per cent of incoming antibiotics but still contributing 17 per cent to river emissions. Decentralised and untreated wastewater systems account for 29 per cent and 54 per cent of antibiotic emissions respectively. Natural processes including instream decay and lake retention eliminated 48 per cent and 13 per cent of antibiotics after discharge.
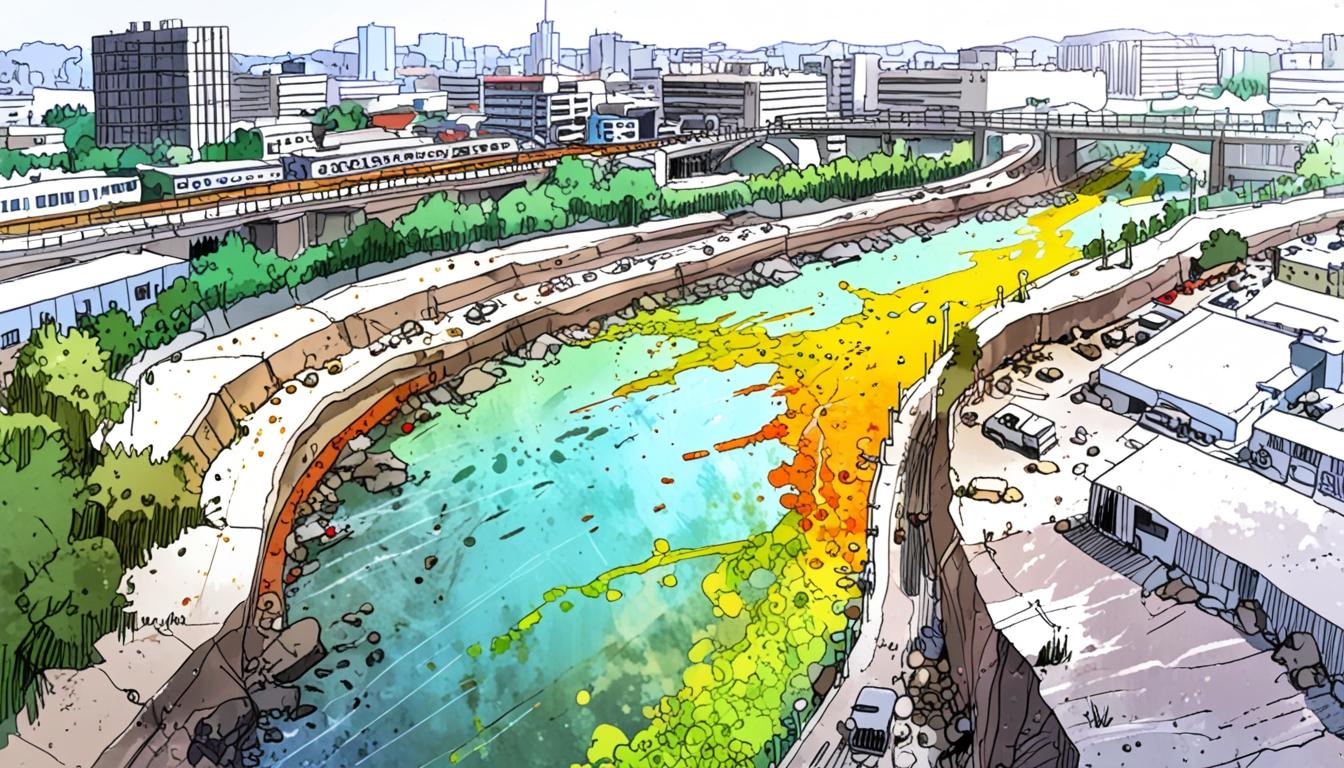
The study assessed environmental exposure using risk quotients calculated as the ratio of antibiotic concentrations in rivers relative to thresholds linked to ecological harm or promotion of AMR. Under low-flow conditions, 49 per cent of river length posed no risk, 9 per cent had low risk, 17 per cent medium risk, and 25 per cent high to very high risk. Notably, about 3.8 million kilometres of rivers contained one or more antibiotics exceeding individual risk limits, while 700,000 kilometres exhibited contamination with ten or more high-risk antibiotics.
Geographically, countries including India, Pakistan, and China were identified as regions with extensive stretches of rivers at high risk. Major contributors to this risk included commonly prescribed antibiotics such as amoxicillin, ceftriaxone, and cefixime. Ciprofloxacin was also a significant factor in some regions, particularly concerning human health exposure.
Regarding direct human exposure to antibiotics through water, the study found that 1.4 per cent of global rivers fall within the highest antibiotic dose percentiles. In scenarios where untreated water is consumed, this exposure potentially affects more than 750 million people.
The researchers emphasised that their model, while focussed on human antibiotic use, likely underestimates overall environmental risks because it does not include veterinary uses, pharmaceutical manufacturing waste, or agricultural runoff. The study acknowledged that seasonal fluctuations and extreme weather events may also cause higher local concentrations than predicted.
Their findings underline the need for improved wastewater treatment systems, more comprehensive regulations governing antibiotic discharge, and prudent use of antibiotics. They suggest prioritising high-risk regions, especially in low- and middle-income countries, through integrated OneHealth strategies that consider human, animal, and environmental health in drug approval and management policies.
This study provides critical insight into the pathways and impacts of antibiotic pollution in freshwater systems globally, reinforcing concerns about environmental contamination’s role in fostering antimicrobial resistance and ecological decline.
Source: Noah Wire Services