In recent years, the biomedical research community has increasingly turned to organoids as a promising alternative to traditional animal models. Organoids are miniature, three-dimensional cellular structures that mimic the architecture and function of human organs, derived from pluripotent stem cells or adult stem cells found in tissue biopsies. This emerging technology addresses significant challenges in understanding and treating human diseases, especially given that over 90% of drugs that appear effective in animal trials fail during human clinical testing.
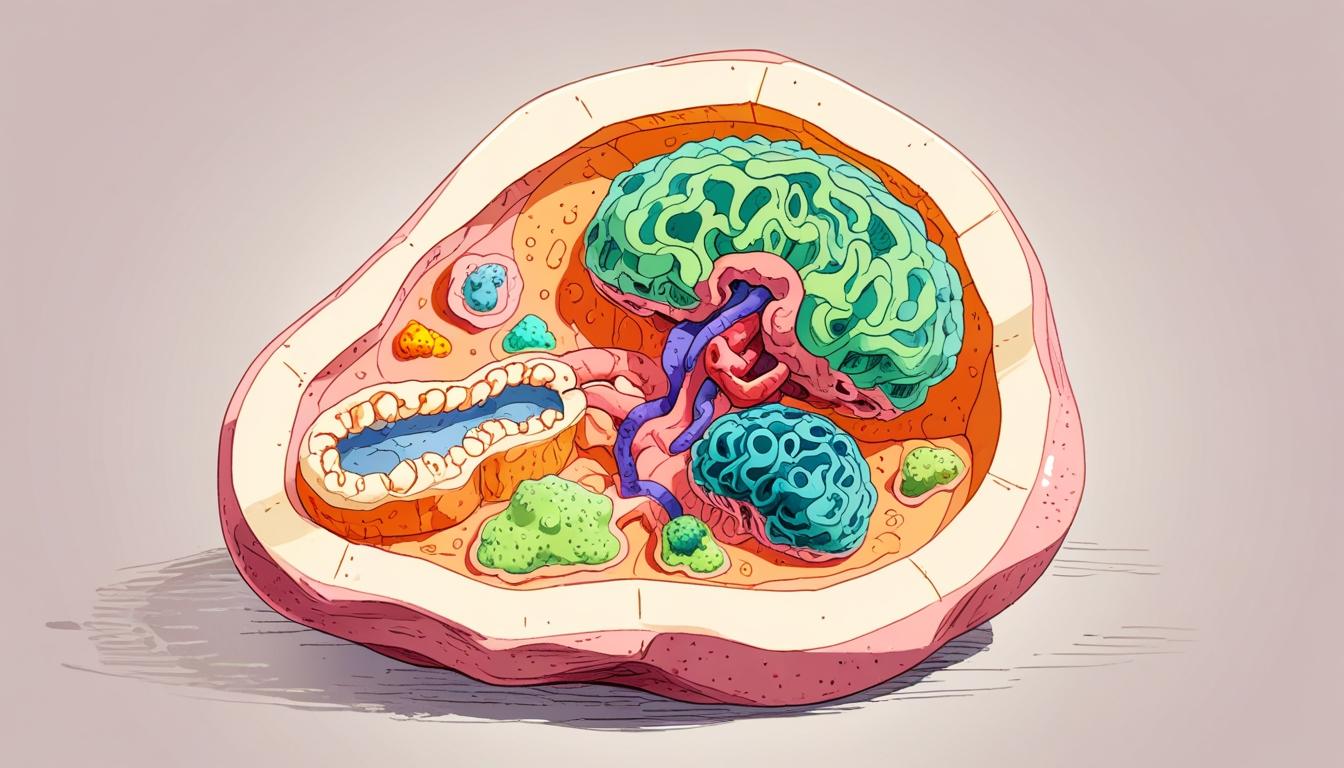
Organoids are created through a meticulous process that guides stem cells using growth factors and mechanical signals to self-organize into complex structures. These models exhibit varying levels of complexity, depending on the organ they are intended to simulate, such as brain, liver, or intestinal organoids. The diversity of cell types within each organoid enables them to replicate specific organ functions and contexts.
One of the primary applications of organoids lies in disease modelling and drug testing. For instance, brain organoids have played a crucial role in understanding the neurodevelopmental impacts of the Zika virus, providing insights previously unattainable through traditional murine models. Similarly, organoids derived from patient-specific intestinal tissues have been used to predict therapeutic responses in individuals with cystic fibrosis. These developments underscore organoids’ potential in enhancing personalized medicine by tailoring treatments to specific patient profiles.
Despite these advantages, organoids have limitations. They lack the complex systemic interactions, such as hormonal regulation and immune responses, that exist in whole organisms. Consequently, while they can replicate certain human-specific disease processes, organoids cannot fully mimic the physiological dynamics necessary for studying chronic diseases or systemic drug effects.
The shift toward organoid use is bolstered by changes in the regulatory landscape. The FDA Modernization Act 2.0, enacted in 2022, encourages the use of validated non-animal testing methods, paving the way for broader adoption of organoids in preclinical research. Companies like Hubrecht Organoid Technology and Emulate Inc. are integrating organoid models into their drug development pipelines, signalling a growing industry confidence in this technology.
Investment in organoid research is also on the rise, fueled by venture capital and public-private partnerships focusing on oncology, gastrointestinal diseases, and neurology. This financial backing highlights the potential for organoids to become a scalable and ethically favourable alternative to animal models in drug testing and disease modelling.
Looking to the future, the integration of organoids with advanced technologies, including gene editing and organ-on-chip systems, may enhance their applicability. Collaborative initiatives, such as the Human Cell Atlas, aim to develop standard protocols and facilitate cross-disciplinary research, further advancing the use of organoids in biomedical science.
In summary, while organoids are not yet poised to entirely replace animal models, they represent a significant advancement in research methodologies. Their ability to provide insights into human-specific biology and therapeutic responses places them as a pivotal tool in the ongoing evolution of biomedical research. As this field continues to develop, the integration of organoids with traditional models and advanced computational techniques may ultimately lead to more efficient drug development and improved patient outcomes.
Source: Noah Wire Services