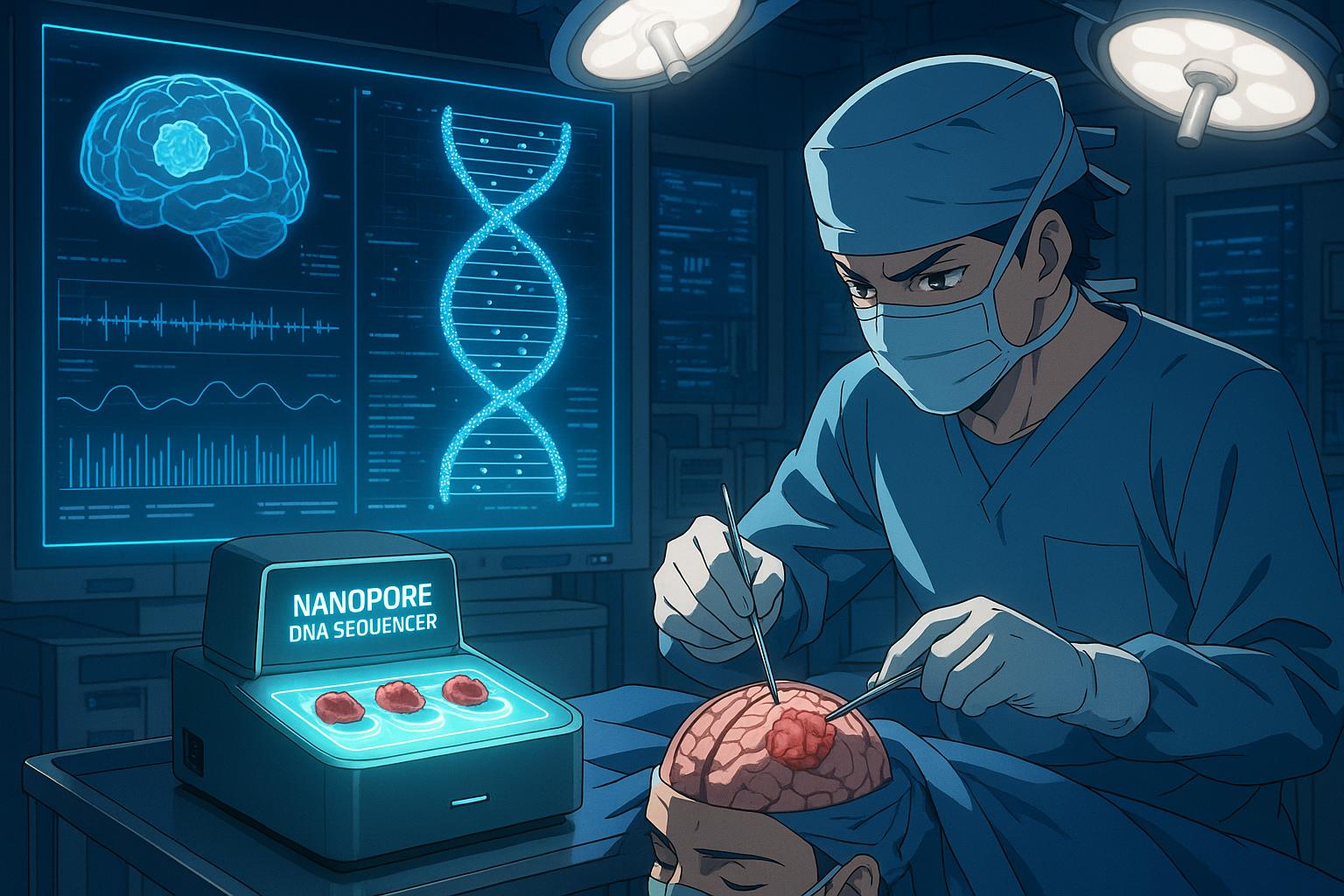
A groundbreaking method for diagnosing brain tumours promises to drastically reduce the wait for patients needing treatment, transforming a process that currently takes weeks into one that could be completed in mere hours. Researchers from the University of Nottingham have developed this innovative technique, which leverages nanopore technology to enable quicker, more accurate diagnostic results.
Globally, around 740,000 individuals are diagnosed with a brain tumour each year, with approximately 50% classified as non-cancerous. Traditional diagnostic pathways involve taking a tumour sample during surgery, which is then studied by pathologists before being subjected to genetic testing. This crucial process often incurs significant delays, especially in the UK, where the wait for genetic testing results can extend to eight weeks or more. Professor Matthew Loose, co-author of the research, emphasised the critical need for timely genetic testing, stating, “Almost all of the samples will go for further testing anyway. But for some of them, it will be absolutely crucial because you won’t know what you’re looking at.”
The researchers’ work, published in the journal Neuro-Oncology, details how they have harnessed nanopore technology to abbreviate diagnostic timeframes substantially. This cutting-edge method employs devices with membranes featuring tiny pores through which an electric current flows. As DNA enters the pore, it is “unzipped” into single strands, and as each strand passes through, it disrupts the current in a unique pattern. This disruption allows the DNA sequence to be read, facilitating real-time classification against known brain tumour markers.
The costs associated with this diagnosis are notably competitive, estimated at around £400 per sample, comparable to traditional genetic testing methods. Initial trials demonstrate a promising level of accuracy; for instance, 80% of the previously extracted samples and 90% of samples taken during surgery were correctly classified within 24 hours. Most strikingly, 76% of the newly collected samples were confidently classified within just one hour. This time efficiency could mean that surgeons could have access to crucial diagnostic information a mere two hours after removing a tumour.
Loose highlighted the importance of this rapid testing capability, which may not only facilitate timely discussions regarding patient treatment in the context of surgical teams but could also directly inform the type of surgery performed on a patient during their operation. Furthermore, the potential exists for this innovation to allow targeted drug delivery during surgery if a specific tumour type is swiftly identified.
This shift towards quicker diagnoses could have broader implications as well. Rapid identification may expedite patient recruitment for clinical trials, enhancing the progression of new therapeutic options. Dr Matt Williams, a consultant oncologist at Imperial College Healthcare NHS Trust, noted the advancement as a positive step, although he cautioned that the effectiveness of faster diagnoses will depend on how they can be integrated into existing treatment protocols. He remarked, “At the moment, intra-operative treatments don’t really exist, although several groups are working on it. But if we want to unlock these approaches, we need to be able to make those diagnoses in the operating theatre to then be able to deploy these treatments.”
The developments in nanopore technology not only have the potential to revolutionise brain tumour diagnostics but are also part of a broader trend in healthcare aimed at improving treatment response times. Similar technology is being employed in various projects, including partnerships with agencies like Genomics England, aimed at speeding up the diagnosis of severe respiratory infections in an effort to prepare for future pandemics. These interdisciplinary applications demonstrate the versatility and promise of nanopore sequencing technology in various medical contexts, spotlighting its emerging role in enhancing patient care and outcomes.
A significant advance in this field has already been observed with other studies demonstrating the effectiveness of rapid diagnostics. One recent study in Nature Medicine achieved tumour classification within 15 minutes, showcasing the possible real-time application of these techniques in surgical settings, while another validation of workflow achieved rapid classification of central nervous system tumours in under 30 minutes. These findings collectively highlight a trend toward more immediate and actionable diagnostics, moving medicine closer to the goal of individualised treatment strategies.
As the implementation of this revolutionary diagnostic method progresses, there remains a clear expectation of not just improved patient experiences but potentially transformative impacts on treatment outcomes for brain tumour patients across the globe.
Reference Map
- Paragraphs 1, 2, 3, 4
- Paragraphs 5, 6
- Paragraph 7
- Paragraph 8
- Paragraph 9
- Paragraph 10
- Paragraph 11
Source: Noah Wire Services