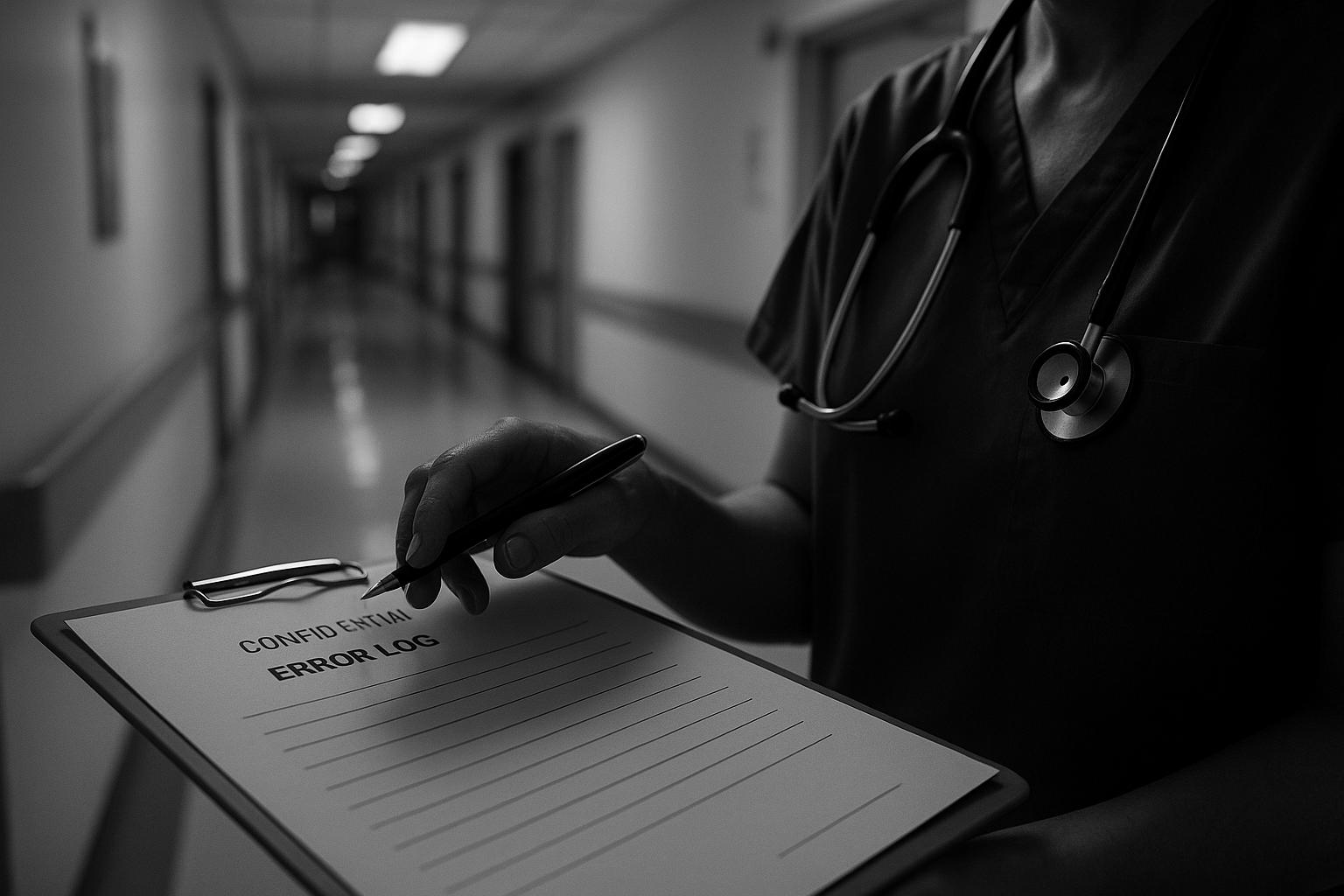
Harm to mothers and their babies within the NHS is under serious threat due to what has been described as a “toxic” culture of cover-up and fear, according to the chief executive of the General Medical Council (GMC). Charles Massey warned that this dangerous environment — where trainee doctors feel hesitant to escalate patient concerns to senior medics — undermines patient safety, especially in maternity care, one of the highest-risk areas of medicine.
In a speech to the Health Service Journal patient safety congress in Manchester, Massey highlighted GMC data showing that more than one in four (27%) obstetrics and gynaecology trainees admit they have felt reluctant to escalate a patient's care to a more senior doctor. This figure is notably higher than in other specialties, pointing to a particularly acute problem within maternity services. The GMC findings also reveal that this specialty experiences above-average rates of workload stress, bullying, and feelings of being unsupported, creating a culture where patient safety is compromised.
Massey described the medical profession as “notoriously tribal,” suggesting that this entrenched division can pit doctors and other healthcare staff against one another, discouraging openness and honesty. He stated, “That doctors are making life and death decisions in environments where they feel fearful to speak up is profoundly concerning.” Such a culture, he added, fosters cover-ups instead of candour, leading to the very outcomes the NHS is trying to prevent: harm to mothers and babies.
The dangers of this culture are reflected in recent high-profile maternity scandals. Families affected have often described themselves as being “gaslit” in their attempts to uncover the truth about their care, according to Health Secretary Wes Streeting, who has launched a national maternity investigation into systemic failures across NHS trusts. The investigation, currently underway, includes a targeted look at trusts of greatest concern—such as those in Leeds and Gloucester—and a broader system-wide review aiming to unify lessons from past inquiries and deliver decisive actions to improve maternity and neonatal care.
Senior midwife Donna Ockenden is also overseeing separate inquiries into maternity deaths and injuries at Nottingham University Hospitals Trust and following up on her previous review of deaths at Shrewsbury and Telford Hospital NHS Trust. These investigations underscore the widespread nature of failures linked to toxic workplace cultures, which not only jeopardise patient safety but also erode trust between staff and management.
Echoing the GMC’s findings, other reports have highlighted that over 20% of trainee doctors across UK specialties hesitate to escalate care, with nearly a third of those in high-pressure areas like obstetrics and gynaecology expressing this concern. This hesitancy has been connected to higher burnout rates among junior doctors, emphasising the urgent need for more supportive working environments where medical professionals feel safe to raise concerns without fear of reprisal.
Further evidence of the pervasiveness of these issues comes from NHS Lothian, where an internal investigation found a toxic culture in women’s services marked by widespread distrust between managers and staff. More than a third of frontline maternity workers reported feeling unable to report unethical behaviour due to fear of retaliation. The region’s health service has since issued an apology and pledged to address the cultural failings highlighted.
Meanwhile, midwives across NHS maternity units have drawn stark attention to the dangerous conditions faced in their wards. One report described the situation as a “game of Russian roulette,” with endemic bullying and dangerously low staffing levels turning labour wards into conveyor belts, undermining the quality and safety of care provided to women in labour. This paints a grim picture of a maternity system in need of urgent reforms both culturally and operationally.
Massey’s call to action stresses the importance of mutual respect, belonging, and inclusion within healthcare teams as prerequisites to safe patient care. He urged employers to create environments where staff feel supported and included, noting that behind troubling statistics are “real people, real tragedies.” The GMC chief concluded with a plea for the NHS to reject cultures that tolerate unsafe care, reinforcing the imperative for change to protect some of the most vulnerable patients—the mothers and babies in maternity wards.
📌 Reference Map:
- Paragraph 1 – [1], [2]
- Paragraph 2 – [1], [3], [4], [5]
- Paragraph 3 – [1], [2]
- Paragraph 4 – [1]
- Paragraph 5 – [1], [3], [4], [5]
- Paragraph 6 – [6]
- Paragraph 7 – [7]
- Paragraph 8 – [1], [2]
Source: Noah Wire Services