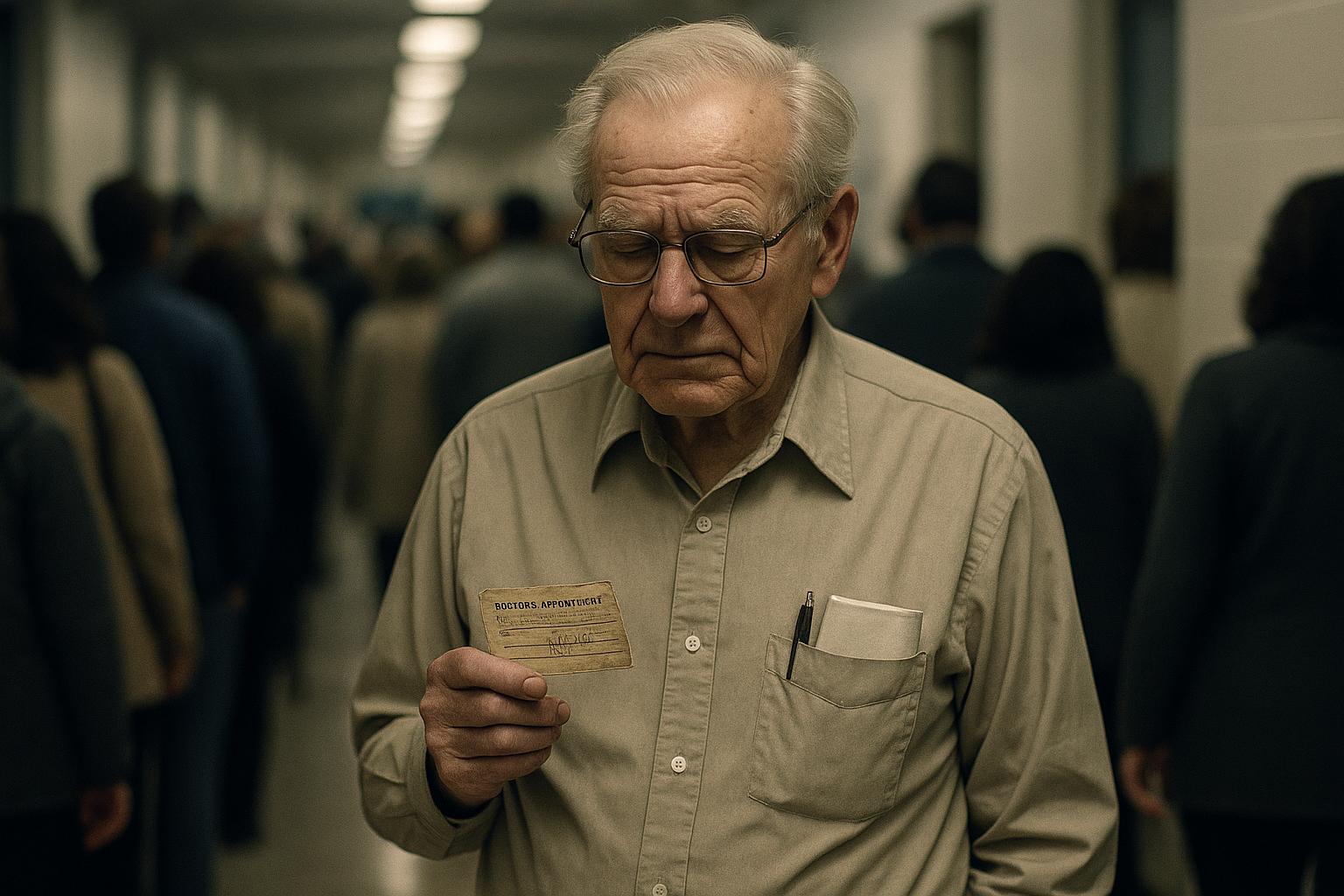
More than three quarters of men in England would attend a prostate cancer screening programme if invited, according to a recent survey commissioned by Healthwatch England. The poll, conducted by Savanta and involving 3,575 men over the age of 18, found that 79% expressed willingness to participate in such a programme. Support was particularly strong among men aged 65 to 74, those who described themselves as financially “very comfortable,” and Black men—groups known to be at higher risk of developing prostate cancer. However, the survey also revealed lower support among those experiencing financial hardship.
Currently, the only screening test available is the prostate-specific antigen (PSA) blood test, which is used primarily when a general practitioner (GP) suspects prostate issues, including cancer. Men over 50 can request a PSA test through their GP, even without symptoms. Yet, routine PSA screening is not offered across the NHS, and national guidance does not recommend a formal screening programme, mainly due to concerns around test accuracy and potential harms.
The survey found that 36% of men over 50 had requested a PSA test, while 60% had not; notably, 7% of those who asked were refused the test. Louise Ansari, chief executive of Healthwatch England, highlighted the importance of clarifying guidance around PSA testing and called for policymakers to consider men's preferences alongside clinical and economic evidence in decisions regarding a national screening policy. She urged the NHS to ensure men can discuss the benefits and risks of prostate cancer testing with their GPs.
Prostate Cancer UK has been campaigning vigorously for the introduction of a national screening programme, emphasising that prostate cancer remains the only major cancer in the UK without one. Amy Rylance, assistant director of health improvement at Prostate Cancer UK, noted that their £42 million TRANSFORM trial is underway to identify the safest and most effective methods for screening. Funded partly by £16 million from the government, this large-scale study aims to provide robust evidence on screening approaches, including combining PSA testing with MRI scans, and is expected to deliver results that could shape policy decisions in the near future. The trial also seeks to address inequalities, particularly the increased risk Black men face from an earlier age.
While enthusiasm builds for national screening, some experts remain cautious about widespread PSA testing, citing mixed evidence from previous long-term studies. The 15-year CAP trial, which involved over 400,000 men aged 50 to 69, showed a small reduction in prostate cancer mortality among those invited for PSA testing but also highlighted significant issues, including overdiagnosis and missed aggressive cancers. Research indicated that one in six prostate cancer diagnoses flagged by PSA screening could be incorrect, raising concerns about potential harms such as unnecessary biopsies and overtreatment.
Such findings have contributed to the UK National Screening Committee’s current stance against recommending population-wide PSA screening, emphasising the need for tests that can reliably detect cancers that require treatment. Despite these challenges, recent advances—such as integrating MRI scanning with PSA testing—are seen as promising steps that may mitigate past drawbacks, which is why many GPs support focused screening, especially for high-risk groups. A separate survey of 400 GPs found overwhelming support for targeted screening programmes aimed at men at greatest risk, with 94% agreeing it would improve diagnosis and outcomes. However, the study also revealed gaps in GPs’ awareness of key risk factors, such as the heightened risk for Black men and those with a family history.
In the face of these complexities, patient and public voices appear united in their desire for improved prostate cancer detection through screening, urging health authorities to act swiftly. Healthwatch England and Prostate Cancer UK both make a case for updating NHS guidelines to empower GPs to initiate conversations about prostate cancer screening earlier, from age 45 for those at highest risk. With multiple stakeholders—from researchers to clinicians and advocacy groups—converging on the critical need for effective screening solutions, decisions expected later this year about a national programme could mark a significant shift in men’s health.
📌 Reference Map:
- Paragraph 1 – [1], [2]
- Paragraph 2 – [1], [2]
- Paragraph 3 – [1], [4]
- Paragraph 4 – [4], [3]
- Paragraph 5 – [5], [6]
- Paragraph 6 – [7], [3]
- Paragraph 7 – [1], [2], [3]
Source: Noah Wire Services