As the autumn season unfolds, the UK is witnessing an unsettling rise in respiratory infections, signalling a potentially challenging winter ahead. Cases of common colds, flu, and Covid-19 are all increasing at a rate that has health officials concerned. According to recent UK Health Security Agency (UKHSA) data based on hospital patient swabs, there has been a one-third increase in common cold virus cases in England within just a week. Meanwhile, hospital admissions due to Covid-19 have surged by 60 percent in a single month from mid-August to mid-September. Adding to the concern, influenza A—the most dangerous strain—is now circulating, with early signs suggesting a harsher flu season is imminent.
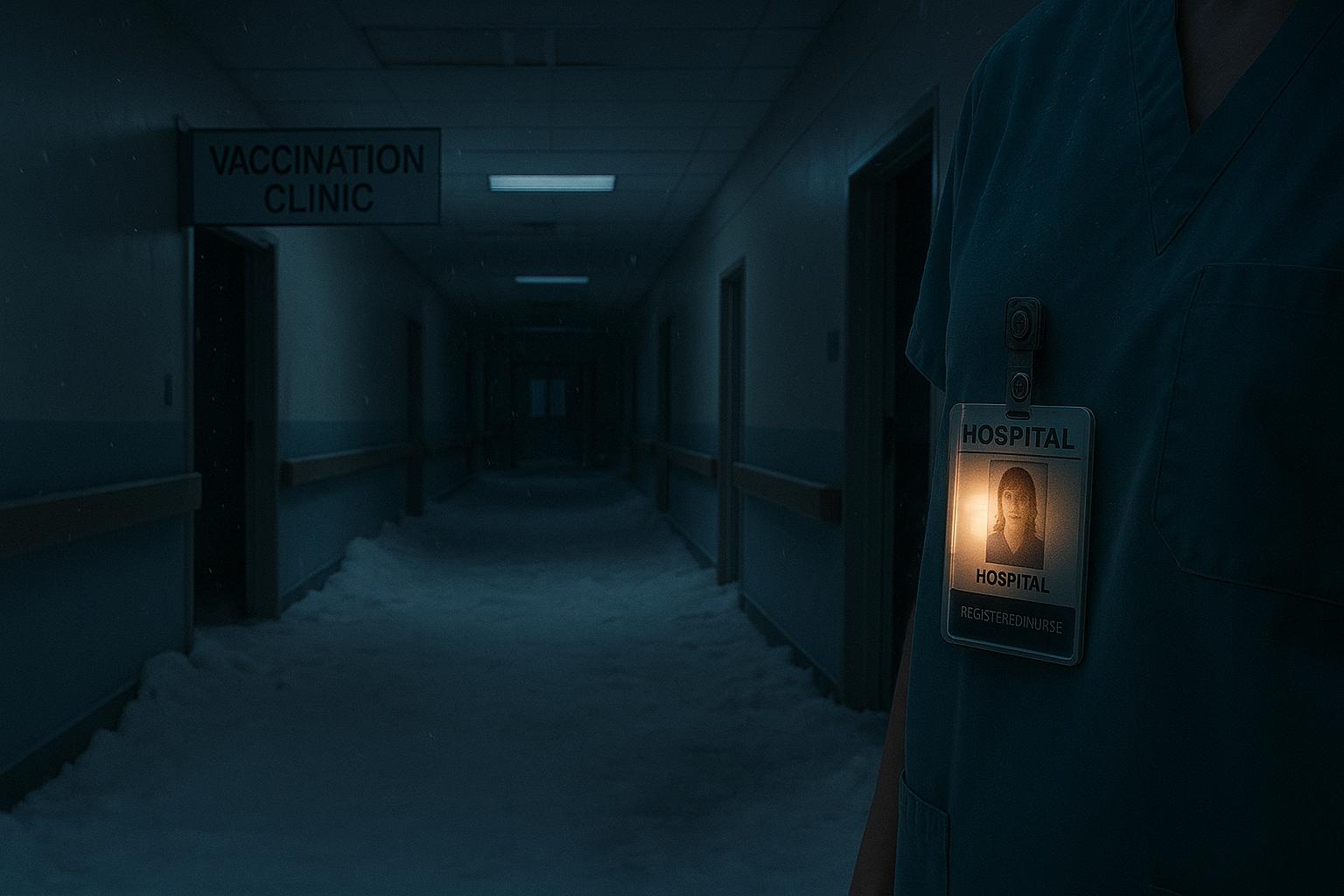
This rise in respiratory illnesses coincides with a vaccination rollout that is still in its early stages this year, a situation health experts have described as "concerning." The pattern echoes warnings from last flu season in the southern hemisphere, especially Australia, where flu cases skyrocketed to more than 400,000, a sharp increase from previous years. Virologists, including emeritus professor John Oxford from Queen Mary University of London, warn that the northern hemisphere could face a similarly severe flu season, although outcomes will depend on additional factors such as vaccine uptake and public health measures.
The current Covid variants, named Stratus and Nimbus, are particularly noteworthy. They present a distinctive symptom—a razor-blade sore throat—alongside the more traditional symptoms such as cough, headache, runny nose, and fever. These strains may also be more easily transmissible than previous ones, raising concerns about the extent of undetected infections since testing mainly captures hospitalised cases, leaving the community spread somewhat invisible.
Another respiratory virus causing alarm is the respiratory syncytial virus (RSV), which is responsible for a substantial number of GP visits, hospitalisations, and deaths, especially among infants and the elderly. Cases of RSV are reported to have increased by around 33 percent in a week, with experts noting that while RSV usually peaks later in the season around November, the advance rise should prompt early preventive measures.
While colds themselves generally cause mild illness, the simultaneous and rapid increase in multiple respiratory viruses raises the risk of sequential infections or secondary bacterial complications, such as pneumococcal pneumonia, particularly following flu or Covid. Professor Peter Openshaw, a respiratory physician at Imperial College London, stresses the importance of starting prevention efforts immediately because virus activity often overlaps as the season progresses.
In light of these developments, vaccinations remain the cornerstone of protection against severe illness. The annual Covid and flu vaccination programme began on October 1, prioritising older adults, care home residents, and individuals with risk factors such as asthma. The Covid vaccine, while not an absolute barrier to infection, has demonstrated effectiveness—in recent US data, it reduced hospitalisation risk by about half in the initial two months post-vaccination. Uptake, however, remains below targets, hampered by vaccine fatigue and scepticism despite evidence affirming the vaccines' safety and efficacy. Similarly, the flu vaccine is recommended, especially for vulnerable groups, with the 2025 vaccine showing promising effectiveness by halving the typical rates of flu-related outpatient visits and hospitalisations observed in the southern hemisphere's recent season.
RSV vaccines have also emerged as a promising new tool, currently available for those aged 75 to 79 and shown to reduce hospital admissions by 72 percent in studies. The limited age range for RSV vaccination has sparked calls for broader availability to better protect the at-risk population.
Complementing vaccination, health experts advocate for continued public health measures such as mask-wearing in crowded settings, hand hygiene, and improved ventilation indoors. A comprehensive review published last year demonstrated that masks significantly reduce transmission not only of Covid but other respiratory viruses as well, with higher-grade respirators offering enhanced protection. Good ventilation practices, including regular airing of indoor spaces, can also limit airborne virus transmission.
Vitamin D supplementation during autumn and winter is advised by the government as a modest immune booster, although its efficacy in preventing colds remains unproven. Nasal sprays and barrier preventatives have mixed reviews, with some products showing potential to reduce severity of respiratory infections by trapping and neutralising viruses in the nasal passages, but others lacking robust clinical backing.
Should infection occur, rest, hydration, and symptom management with basic analgesics like paracetamol or ibuprofen are recommended, while antibiotics remain appropriate only for secondary bacterial infections. The availability of at-home Covid and flu tests is a valuable tool for prompt diagnosis, helping individuals isolate to reduce spread.
In sum, the early surge in multiple respiratory viruses, combined with ongoing vaccine hesitancy and delayed immunisation, points to a winter season where vigilance and proactive health behaviours are essential. Authorities urge the public to embrace vaccination and basic preventative measures to mitigate the impact of what could prove to be one of the most severe cold and flu seasons in recent years.
📌 Reference Map:
- Paragraph 1 – [1], [2], [7]
- Paragraph 2 – [1], [2], [3]
- Paragraph 3 – [1], [3]
- Paragraph 4 – [1], [3]
- Paragraph 5 – [1], [3]
- Paragraph 6 – [1], [3]
- Paragraph 7 – [1], [3]
- Paragraph 8 – [1], [3], [7]
- Paragraph 9 – [1], [3]
- Paragraph 10 – [1], [3]
- Paragraph 11 – [1], [3]
- Paragraph 12 – [1], [3]
Source: Noah Wire Services