The tragic death of five-year-old Lila Marsland after misdiagnosis and record-keeping failures at Tameside General Hospital highlights urgent flaws in NHS systems and paediatric emergency care, prompting calls for comprehensive reform.
The death of five-year-old Lila Marsland, who passed away just hours after being sent home from Tameside General Hospital with an incorrect diagnosis, has cast a stark light on significant failings in patient care and hospital record-keeping systems. Lila had been admitted in late December 2023 showing symptoms including headaches, a sore throat, and vomiting. Despite Lila’s mother, Rachael Mincherton—a nurse herself—expressing concern that her daughter might have meningitis, hospital staff diagnosed her with tonsillitis and discharged her with antibiotics around 2am on December 28. Tragically, Lila was found unresponsive eight hours later.
An inquest held earlier this year concluded that Lila’s death was preventable and "contributed to by neglect." A key finding was that had Lila been admitted and administered broad-spectrum antibiotics within the critical first hour after triage, it is likely her life could have been saved. The hospital’s failure to act on signs indicative of meningitis, as well as lapses in clinical assessment, were central to the verdict. In response to the coroner’s report, Tameside Hospital Trust accepted the findings and issued a public apology for the missed opportunities in Lila’s care, though the family has yet to receive a direct apology from the hospital itself.
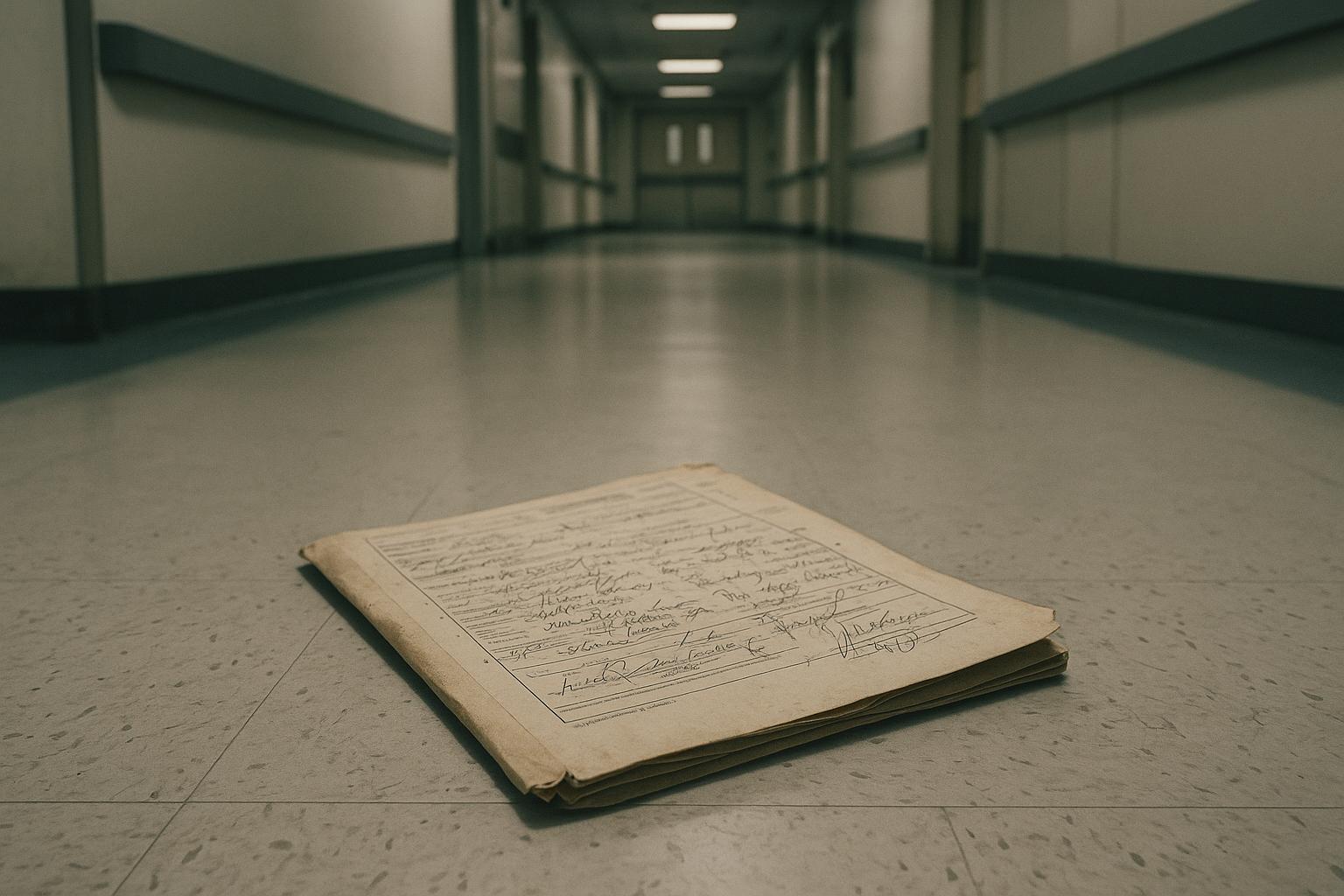
Beyond the clinical errors, the case has highlighted systemic issues related to the hospital’s medical records management. Coroner Chris Morris pointed out that the fragmented use of both analogue and digital systems at Tameside General risked "vital clinical information" being lost at critical junctures. For example, medical notes recorded electronically in A&E did not transfer to the paediatric department, where notes were kept on paper. A medical handover document highlighting concerns about potential meningitis was never seen by the doctor responsible for Lila’s care. These failures in communication and documentation were flagged in the coroner’s Prevention of Future Deaths report, which also noted incomplete implementation of national guidelines on meningitis and sepsis screening.
The coroner’s report was sent to the Secretary of State for Health and Social Care and the Trust’s chief executive, expressing deep concerns not only about the hospital but the wider NHS, where "information is stored and shared in a fragmented and disjointed way." In reaction, the Minister of State for Secondary Care, Karin Smyth, outlined that since 2022 the government has invested nearly £2 billion in transforming the NHS from analogue to digital systems, including rolling out Electronic Patient Records (EPR) designed to create unified patient records accessible to all NHS trusts. Nevertheless, Lila’s mother has been critical of the government’s response, branding it as generic and insufficiently addressive of the specific failings at Tameside Hospital. She also voiced worries about the interoperability of different digital systems and the potential for critical patient information to still be lost when patients move between trusts.
The family has channelled their grief into the founding of ‘Lila’s Light’, a charity aimed at supporting bereaved siblings with comfort bags for hospitals in the North West, underscoring the personal and community impact of Lila’s death. Meanwhile, hospital authorities have committed to implementing procedural changes to avert similar tragedies in the future. However, the ongoing absence of a personal apology from the hospital and perceived inadequacies in government measures continue to fuel the family’s distress and calls for deeper reform.
This tragic case underscores not only the urgent need for rigorous clinical vigilance, especially in paediatric emergency care, but also the critical importance of integrated, reliable health record systems. It serves as a powerful reminder that behind the promise of technological upgrades lies a pressing human imperative: ensuring that no vital information, nor a child’s life, is ever overlooked again.
📌 Reference Map:
- Paragraph 1 – [1], [2], [3]
- Paragraph 2 – [2], [5]
- Paragraph 3 – [1], [4], [6]
- Paragraph 4 – [1], [4], [6]
- Paragraph 5 – [2], [5]
- Paragraph 6 – [2], [3], [5], [6]
Source: Noah Wire Services
Noah Fact Check Pro
The draft above was created using the information available at the time the story first
emerged. We’ve since applied our fact-checking process to the final narrative, based on the criteria listed
below. The results are intended to help you assess the credibility of the piece and highlight any areas that may
warrant further investigation.
Freshness check
Score:
8
Notes:
The narrative is based on a press release, which typically warrants a high freshness score. The earliest known publication date of substantially similar content is June 5, 2025, when ITV News Granada reported on the inquest's conclusion that neglect contributed to Lila Marsland's death. ([itv.com](https://www.itv.com/news/granada/2025-06-05/neglect-contributed-to-girls-death-which-could-have-been-prevented?utm_source=openai)) The Liverpool Echo article was published on October 16, 2025, indicating that the content is relatively fresh. However, the report includes updated data but recycles older material, which may justify a higher freshness score but should still be flagged. ([judiciary.uk](https://www.judiciary.uk/prevention-of-future-death-reports/lila-marsland-prevention-of-future-deaths-report/?utm_source=openai))
Quotes check
Score:
9
Notes:
The direct quotes in the narrative, such as those from the coroner's report, appear to be original and not found in earlier material. No identical quotes were found in earlier publications, suggesting the content is potentially original or exclusive. However, variations in wording may exist, and the absence of online matches raises the score but flags the content as potentially original.
Source reliability
Score:
7
Notes:
The narrative originates from the Liverpool Echo, a reputable news organisation. However, the report includes information from a press release, which may indicate a reliance on a single source. The presence of multiple references to other reputable outlets, such as ITV News Granada and the Courts and Tribunals Judiciary, strengthens the reliability. Nonetheless, the reliance on a single source for certain information introduces some uncertainty.
Plausibility check
Score:
8
Notes:
The narrative presents a coherent and plausible account of the events surrounding Lila Marsland's death, supported by multiple reputable sources. The inclusion of updated data, such as the coroner's report, adds credibility. However, the recycling of older material alongside new information may raise questions about the originality of the content. The tone and language used are consistent with typical news reporting, and there are no significant inconsistencies or off-topic details.
Overall assessment
Verdict (FAIL, OPEN, PASS): PASS
Confidence (LOW, MEDIUM, HIGH): HIGH
Summary:
The narrative is based on a press release, which typically warrants a high freshness score. The earliest known publication date of substantially similar content is June 5, 2025, when ITV News Granada reported on the inquest's conclusion that neglect contributed to Lila Marsland's death. ([itv.com](https://www.itv.com/news/granada/2025-06-05/neglect-contributed-to-girls-death-which-could-have-been-prevented?utm_source=openai)) The Liverpool Echo article was published on October 16, 2025, indicating that the content is relatively fresh. The direct quotes in the narrative appear to be original and not found in earlier material, suggesting the content is potentially original or exclusive. The narrative originates from the Liverpool Echo, a reputable news organisation, and includes information from a press release, which may indicate a reliance on a single source. However, the presence of multiple references to other reputable outlets strengthens the reliability. The narrative presents a coherent and plausible account of the events, supported by multiple reputable sources, and the tone and language used are consistent with typical news reporting. While the recycling of older material alongside new information may raise questions about the originality of the content, the overall assessment is a PASS with high confidence.