The soaring financial burden linked to medical negligence in England’s maternity services spotlights deep-rooted failures within the NHS, reinforcing calls for urgent and systemic improvements. The National Audit Office estimates negligence liabilities now total around £60 billion, a fourfold increase in under two decades. This escalation largely stems from obstetric cases, where payouts tend to be significantly higher due to the lifelong care required for babies who suffer injuries at birth.
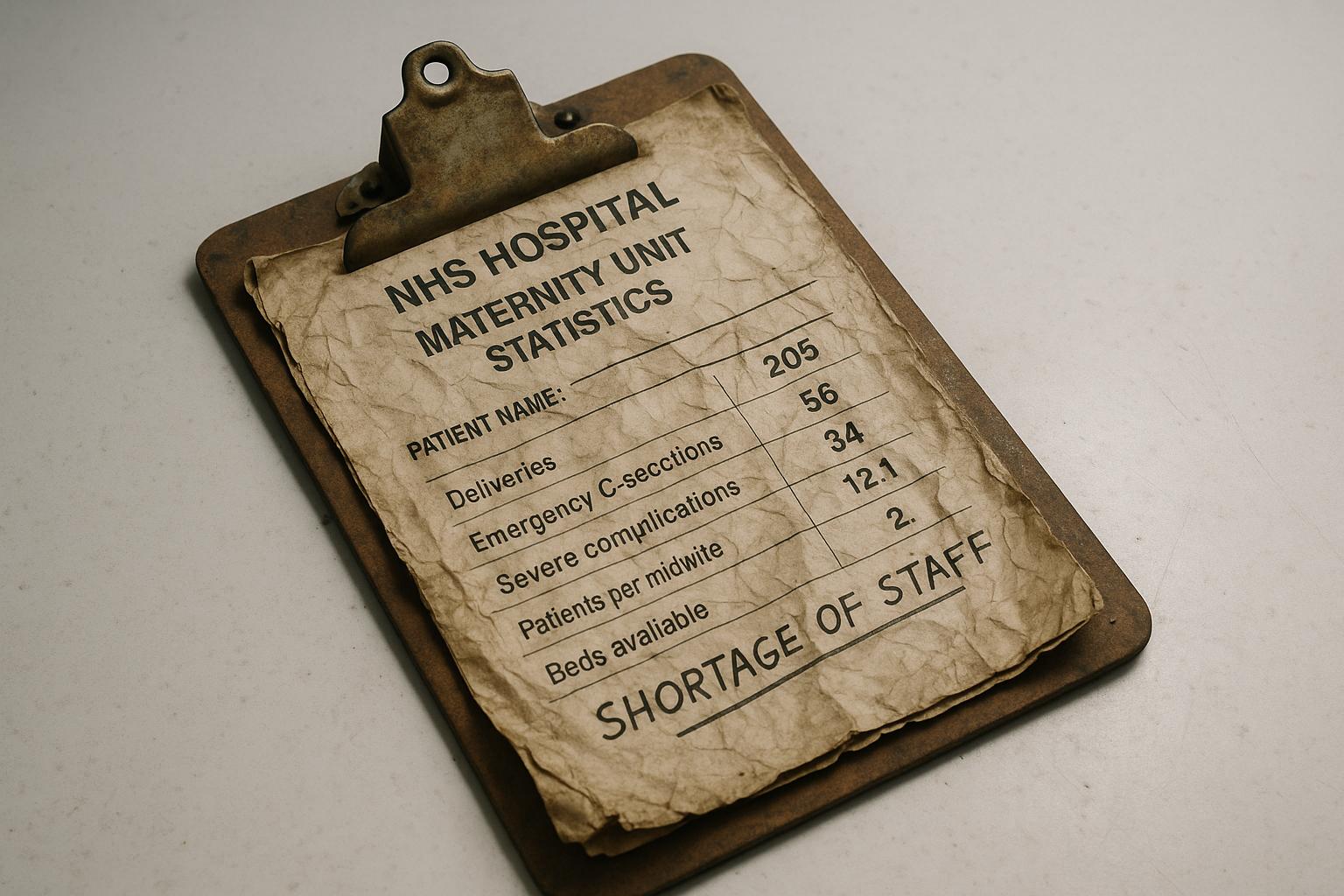
The scale of maternity-related negligence is stark. In 2023/24, the NHS in England spent £2.8 billion on damages and legal costs for clinical negligence claims, with maternity care alone accounting for half that total. Although maternity claims represent only 13% of all clinical claims, they make up 57% of the payout value, underscoring the disproportionate financial impact of birth-related injuries. Such data reflects both the high cost of care for affected infants and the ongoing strain on NHS resources.
This troubling financial picture is mirrored by equally alarming maternity care outcomes. A Care Quality Commission (CQC) review revealed that nearly half of NHS maternity units require improvement or are inadequate. Issues such as unreported serious harm incidents, long delays in clinical assessments, lack of adequate space and equipment, and pervasive discrimination contribute to unsafe environments. Health Secretary Wes Streeting labelled these failings a “cause for national shame,” vowing that raising maternity care standards would be a key test for his administration.
Yet, despite numerous publicised scandals over the years—including tragic failings in Morecambe Bay, Shrewsbury and Telford, East Kent, and more recently Nottingham—the persistence of preventable deaths and injuries highlights systemic problems. Investigations into these cases have repeatedly pointed to weak leadership, poor inter-clinician collaboration, inadequate staffing levels, and an entrenched failure to learn from mistakes. The first parliamentary report on birth trauma reviewed last year condemned the tolerance of substandard care and the perception of women as inconveniences rather than patients deserving of dignity.
The complexity of the challenges is compounded by demographic shifts and evolving clinical demands. The increasing numbers of older and heavier mothers, alongside a higher incidence of caesarean sections, place additional strain on staff and systems. These factors, coupled with unmanageable workloads, contribute to ongoing staff retention difficulties—and by extension, care quality issues.
Financially, the maternity programme’s annual budget of approximately £122 million contrasts sharply with the multi-billion-pound costs arising from clinical negligence claims. Between 2018/19 and 2022/23, the NHS faced over £3 billion in negligence payouts related to obstetrics alone. Some caution surrounds headline figures: fact-checking reveals that annual clinical negligence payments for maternity are closer to £1.1 billion rather than overstated totals sometimes cited; nevertheless, the liability remains profound and unsustainable.
In June 2025, in recognition of these crises, Wes Streeting formally launched an inquiry into maternity services, targeting up to ten of the worst-performing trusts and aiming to produce recommendations by December 2025. This investigation follows decades of scandals and signals a critical government focus on reversing entrenched problems. However, bereaved families and campaigners express scepticism about whether new recommendations will transcend previous failed promises, given the NHS maternity service’s enduring challenges.
Beyond tragic birth injuries and fatalities, indicators such as the rising incidence of severe vaginal tears, increased maternal mortality, and hospital readmissions signal systemic weaknesses that extend to the broader experience of childbirth. Some rise in maternal injuries may reflect improved reporting and awareness in a historically under-discussed area. Nonetheless, rising costs and persistent poor outcomes sharply underline that incremental improvements are insufficient.
Ultimately, the rising payouts for maternity-related negligence cases, alongside continuing reports of unsafe care, serve as urgent warnings. There is no simple fix for the intricate problems facing maternity services, but the government's inquiry and renewed ministerial attention present an opportunity. The key challenge lies in translating recommendations into concrete, lasting improvements to ensure safe, dignified, and equitable care for all mothers and babies.
📌 Reference Map:
- Paragraph 1 – [1], [7], [2], [6]
- Paragraph 2 – [2], [6], [4]
- Paragraph 3 – [3], [1], [5]
- Paragraph 4 – [1], [3], [5]
- Paragraph 5 – [1], [2], [3]
- Paragraph 6 – [4], [6]
- Paragraph 7 – [5], [1], [3]
- Paragraph 8 – [1], [7], [2]
- Paragraph 9 – [1], [5], [3]
Source: Noah Wire Services