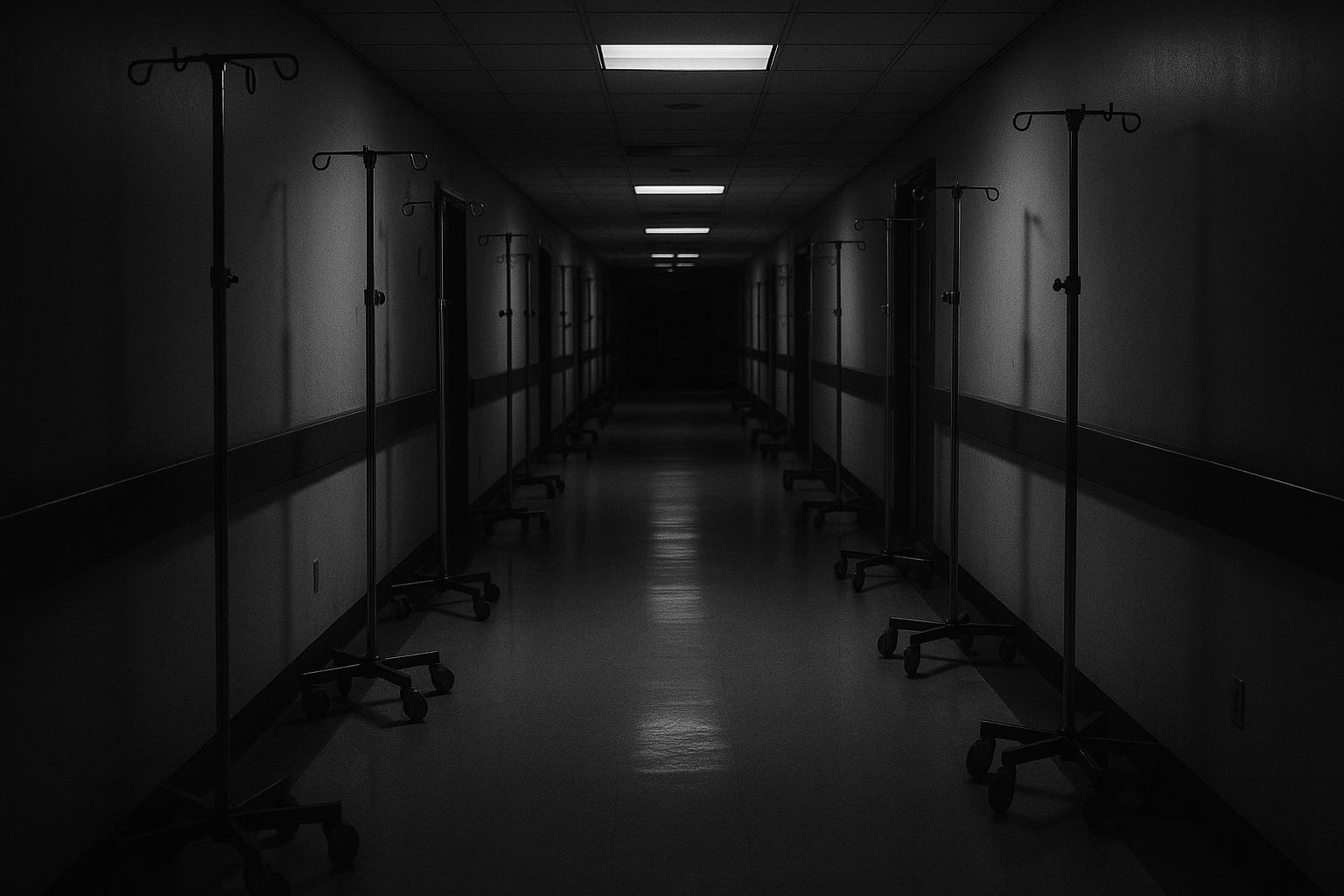
As the UK moves deeper into the autumn months, the National Health Service (NHS) is already grappling with a severe winter crisis, with hospitals across the country overwhelmed by surging numbers of flu and COVID-19 patients. The escalating pressure has pushed healthcare facilities to their limits, with patients being placed in makeshift wards, including converted spaces such as a Costa Coffee café, and even treated in corridors, waiting rooms, cupboards, and offices due to a lack of available beds. Medics describe the situation as unprecedented outside of the peaks observed during the height of the pandemic, warning of an impending period that some are likening to “Armageddon.” The surge has been compounded by an unusually early and aggressive flu season alongside increased demand for emergency care and cuts in staffing, setting the NHS on a precarious trajectory ahead of winter.
The scale of the crisis is striking. From June to September alone, NHS data analysed by the Royal College of Emergency Medicine showed that over 500,000 patients had to stay in A&E for more than twelve hours awaiting admission, a figure surpassing the entire winter period of the previous particularly severe Covid-impacted year. Hospitals are reportedly operating at the highest level of alert (OPEL 4), indicating critical pressure that impedes their ability to deliver safe and comprehensive care. Doctors report that patients often remain in corridors or waiting rooms for days, receiving intravenous treatments where prolonged hospital admission spaces are unavailable. The repeated resort to so-called “corridor care” has become a distressingly routine feature, as highlighted in a summer survey by the Royal College of Physicians which found that 60% of doctors had been forced to care for patients in temporary or inappropriate spaces.
Adding to the strain, there have been alarming reports of cuts in doctors’ shifts and recruitment freezes attributed to financial constraints within NHS trusts. According to medics on the ground, these staffing reductions risk exacerbating the crisis given rising patient numbers, with some emergency departments experiencing critical shortages amid a wave of flu, Covid, and recently, even measles cases. Staff sickness due to seasonal illnesses compounds the workforce challenge, with key voices in the medical community warning that the system’s capacity to respond effectively is being undermined just as demand peaks.
This year’s difficulties follow what was described as a “bad” summer for the NHS, with many hospital wards already crippled by demand and limited resources. Experts and leaders in emergency medicine have been sharply critical of government and NHS leadership for what they view as inadequate planning and response to the looming crisis. Dr Ian Higgins, president of the Royal College of Emergency Medicine, expressed frustration that the government had “missed the boat” on meaningful winter preparedness, lamenting the lack of decisive action despite clear signals of increasing pressure over recent months.
The crisis is exacerbated by wider systemic issues such as delayed discharges owing to insufficient social and elder care capacity. Care England’s chief executive highlighted the failure to expand care home bed availability, a move that could otherwise help ease hospital pressures by facilitating more appropriate discharges. This lack of integration and cooperation between NHS and social care sectors continues to fuel bed shortages and contribute to “bed blocking,” which intensifies overcrowding in emergency departments.
Government officials have acknowledged the challenges, with Health Secretary Wes Streeting describing the coming winter as “challenging” but underscoring efforts to prepare, including investing in the construction of new emergency care centres, expanding mental health crisis facilities, and acquiring more ambulances. A Department of Health and Social Care spokesperson also noted the launch of the winter vaccine programme for COVID-19 and flu, emphasising the importance of immunisations as a protective measure for vulnerable groups and the wider healthcare system. Nevertheless, as winter approaches, the urgent concerns voiced by frontline staff expose a critical need for more immediate and effective interventions to safeguard patient care and health service sustainability.
The NHS faces perhaps its sternest test in years as it confronts the dual challenges of infectious diseases, bed shortages, and workforce pressures. Without rapid and comprehensive action to strengthen staffing, improve patient flow, and ensure adequate social care support, the country risks enduring another winter of severe healthcare strain, with dire implications for patient outcomes and system resilience.
📌 Reference Map:
- Paragraph 1 – [1] (The Independent), [2] (The Independent)
- Paragraph 2 – [1] (The Independent), [3] (WSWS), [7] (Royal College of Emergency Medicine)
- Paragraph 3 – [1] (The Independent), [3] (WSWS), [6] (WSWS)
- Paragraph 4 – [1] (The Independent), [5] (Evening Standard)
- Paragraph 5 – [1] (The Independent)
- Paragraph 6 – [1] (The Independent)
- Paragraph 7 – [1] (The Independent), [4] (Healthwatch Halton)
- Paragraph 8 – [1] (The Independent), [5] (Evening Standard)
Source: Noah Wire Services