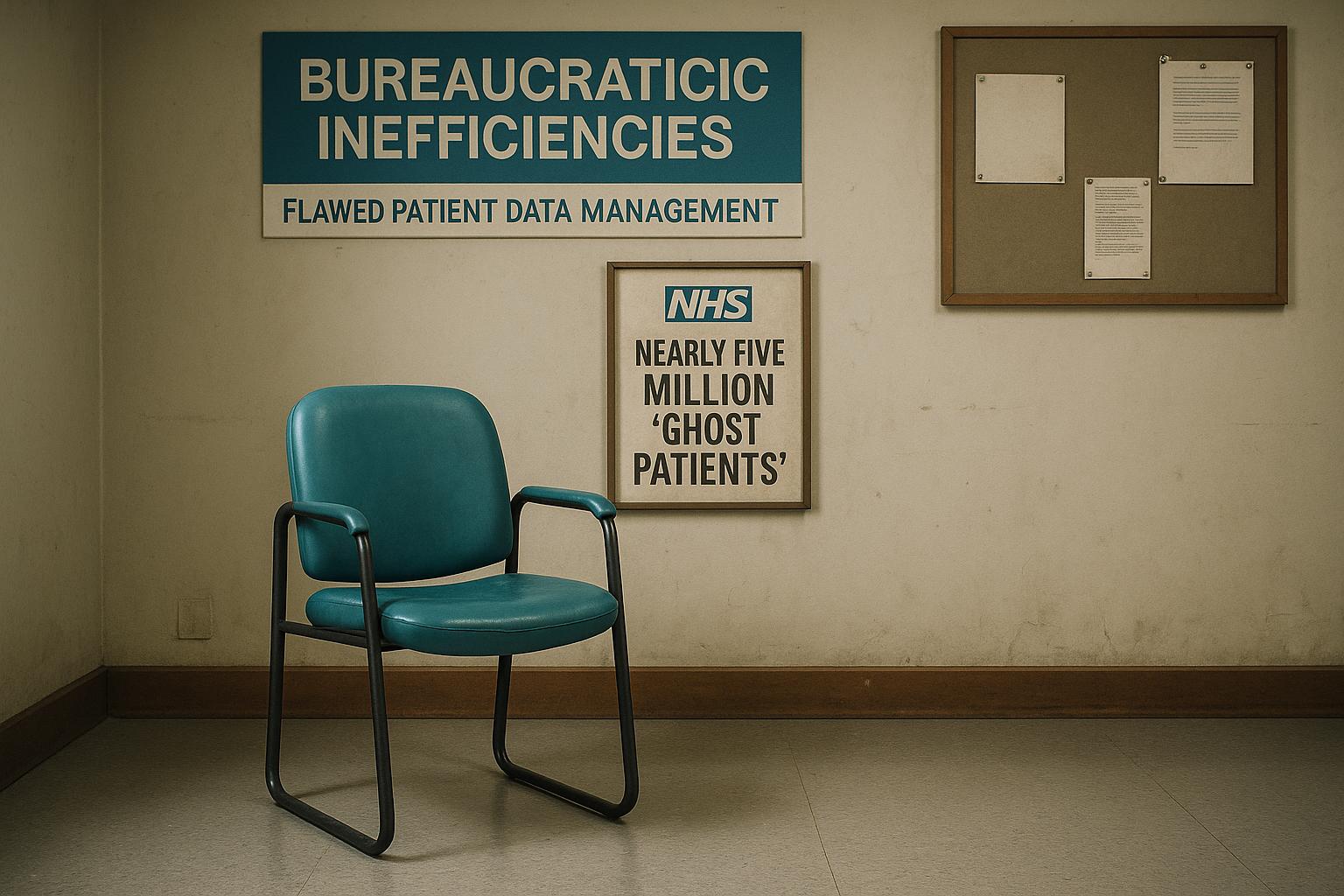
GP surgeries in England are reportedly registering an unprecedented number of 'ghost patients'—individuals who do not exist on their lists but for whom the practices receive payments. According to an investigation by the Daily Mail, almost 5 million such phantom patients are currently registered nationally, marking a 95% increase over the past decade. The total number of registered patients stands at 63.8 million, while the estimated population is closer to 58.8 million, creating a substantial discrepancy that has fuelled concerns about inefficiencies and funding misallocations in the NHS. At an average payment of £169.74 per registered patient, GP practices could be receiving about £838 million annually for non-existent patients, funds that could otherwise be channelled into vital healthcare resources such as nurse training.
This scale of inflation in patient lists is not localized. Parts of England, including North West London and regions like Humber and North Yorkshire, are showing disparities where registered patient numbers exceed actual population estimates by over 20%, with some areas approaching or exceeding 30%. Such wide-ranging discrepancies point to systemic issues rather than isolated cases.
The underlying causes, according to authoritative voices including the Royal College of General Practitioners (RCGP) and the British Medical Association (BMA), stem primarily from records management challenges rather than deliberate financial misconduct by GP practices. Dr Victoria Tzortziou-Brown, Vice Chair of the RCGP, emphasised that maintaining accurate patient lists depends heavily on receiving timely and precise information about patient movements. Without this, list inflation can occur naturally. Similarly, BMA representatives warn against blaming GPs, who are already operating under significant workload pressures, for the presence of ghost patients. They also highlight that government funding levels are inadequate to meet current demands, and inflated lists do not equate to profitable practices.
Investigations into the issue have been periodically conducted. The NHS Counter Fraud Authority began scrutiny in 2019 after detecting anomalies but paused the work due to data challenges and resource shifts during the Covid pandemic. Despite this, there is acknowledgment that a minority of practices might deliberately retain invalid patient records for financial or political reasons, inflating patient-to-GP ratios used in funding and staffing negotiations.
Efforts to remedy the problem include stricter controls introduced in September 2023, such as Primary Care Support England (PCSE), managed by an outsourcing firm, flagging patients potentially no longer at their registered addresses. Practices now have shorter windows to confirm patient status, aiming to improve list accuracy. However, critics argue that the pace of digital transformation within the NHS is slow and that bureaucratic inertia persists, hampering more effective reforms.
Political figures and healthcare analysts alike have voiced frustration over the ongoing challenges. Shimeon Lee of the TaxPayers' Alliance called the situation a 'damning indictment' of NHS bureaucracy, while Sir Geoffrey Clifton-Brown, chair of the Public Accounts Committee, warned that without faster digital progress and cultural change, ghost patients will continue to 'haunt' the healthcare system. The Health Foundation's Dr Luisa Pettigrew noted that discrepancies in patient registration are exacerbated by population mobility and delayed data updates, with some regions experiencing greater mismatches than others.
The fallout touches on wider NHS policy debates as well, with GPs warning of their workload strains amid new requirements for continuous online appointment requests, provoking tensions with government officials over resourcing and safe practice limits.
Regional cases such as those in Hampshire and the Isle of Wight, as well as Nottingham and Nottinghamshire, exhibit similar patterns with tens of thousands of ghost patients inflating patient lists, according to local NHS and census data. In each case, the RCGP stresses that these figures reflect administrative issues rather than any attempt at fraud or profiteering.
Overall, while the monetary sums involved are substantial, the core concern remains the integrity and accuracy of patient data within GP lists. Reliable records are crucial not only for fair funding but also for ensuring that healthcare services are appropriately planned and delivered. Addressing this issue will require sustained technological investment, improved data sharing protocols, and a clearer prioritisation of digital transformation within the NHS framework.
📌 Reference Map:
- Paragraph 1 – [1] (Daily Mail), [2] (Independent), [3] (Standard), [7] (Irish News)
- Paragraph 2 – [1] (Daily Mail), [5] (Alton Herald), [6] (Worksop Guardian)
- Paragraph 3 – [1] (Daily Mail), [4] (RCGP), [1] (Daily Mail - BMA comments)
- Paragraph 4 – [1] (Daily Mail - NHS Counter Fraud Authority), [1] (Daily Mail)
- Paragraph 5 – [1] (Daily Mail - PCSE system and reform), [1] (Daily Mail - political commentary)
- Paragraph 6 – [1] (Daily Mail - Political and health think tank quotes), [4] (RCGP)
- Paragraph 7 – [5] (Alton Herald), [6] (Worksop Guardian), [4] (RCGP)
- Paragraph 8 – [1] (Daily Mail), [4] (RCGP)
Source: Noah Wire Services