Stroke patients and others requiring intensive physiotherapy are facing a decline in care quality, largely due to inadequate rehabilitation space and equipment within NHS hospitals, according to a recent survey by the Chartered Society of Physiotherapists. The poll, which included over 2,000 NHS physiotherapy staff, revealed that four in ten have lost, or are at risk of losing, dedicated rehabilitation areas. Additionally, six in ten reported that their therapy rooms had been repurposed by other clinical teams, often citing insufficient funding or a lack of managerial prioritisation as underlying causes.
Sara Hazzard, assistant director of the society, expressed deep concern over the ongoing erosion of rehabilitation spaces. She highlighted the critical importance of these areas, where patients recover mobility and rebuild their lives following strokes or surgeries. Hazzard urged the government to enforce NHS England’s existing estates guidance more rigorously, warning that without restoring and protecting these facilities, the government’s broader ten-year strategy to deliver care closer to home may falter, leaving vulnerable patients behind.
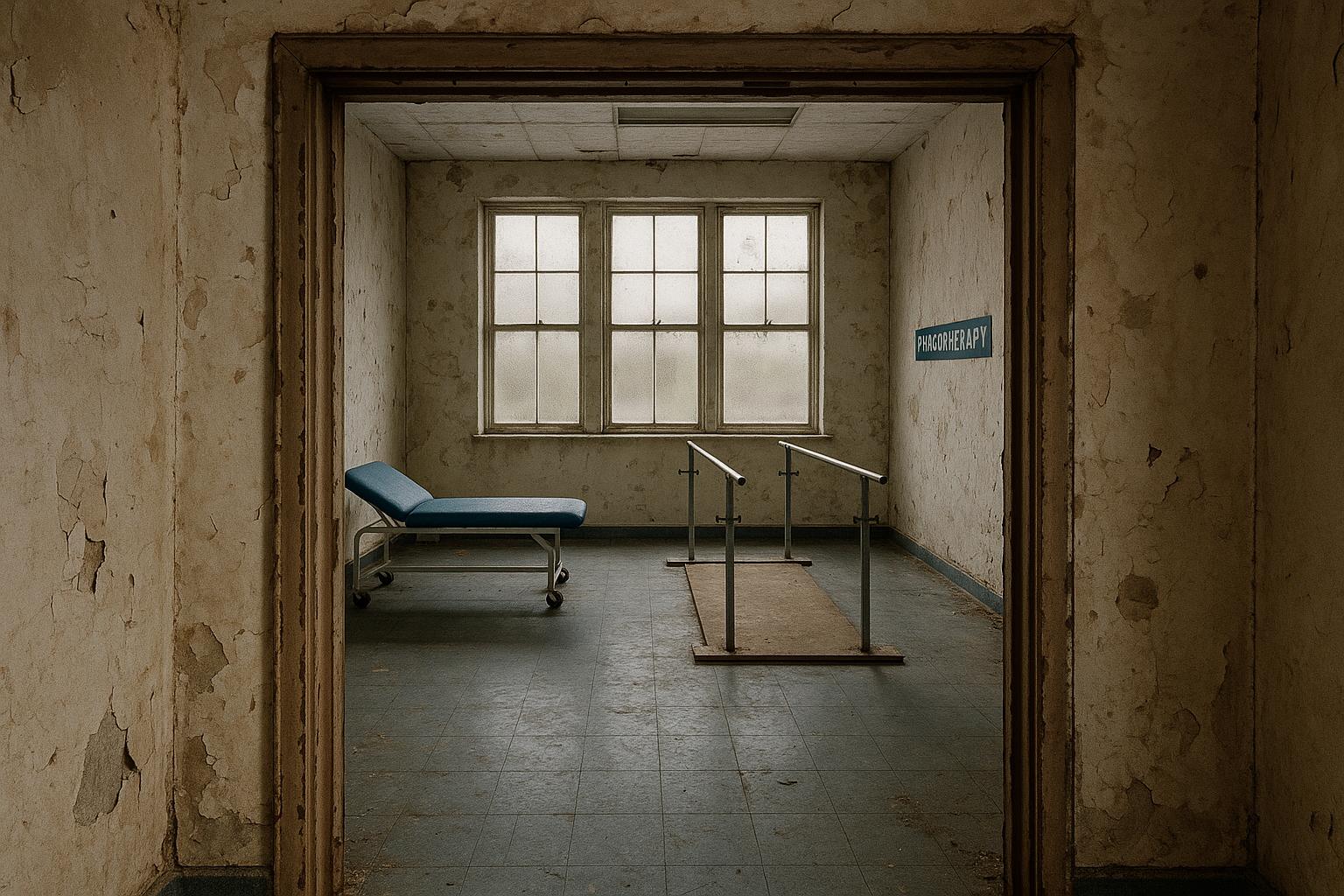
A striking example from a physiotherapist working in stroke rehabilitation illustrated the consequences of this decline: their therapy gym had been reduced to a mere 15 square metres. This severe spatial limitation meant none of their stroke patients achieved the recommended three hours daily of supervised movement and group activities, vital for recovery. The therapist emphasised that with increased space and staffing, these rehabilitation targets could be met, framing the current situation as a matter of chance rather than consistent care.
The survey outcomes painted a troubling picture of NHS physiotherapy services nationwide. Nearly three-quarters of staff reported a decline in rehabilitation quality, while over half experienced reduced access to essential equipment. More than half noticed an increase in patient disability levels and a higher likelihood of hospital readmissions among those they treated. One physiotherapist highlighted the distress felt by patients recovering from falls, noting that busy wards are ill-suited for the sensitive physical and mental recovery these individuals require.
These findings reflect broader systemic challenges. A 2022 survey found that the COVID-19 pandemic had already caused significant disruptions to physiotherapy services, with 73% of physiotherapists unable to provide adequate care due to space being repurposed, forcing treatment into corridors and storage areas. Such conditions led to extended patient waiting times and compromised rehabilitation effectiveness. Similarly, a 2024 report by the British Geriatrics Society documented significant inequalities in rehabilitation services for older adults across the UK, where resource shortages and restrictive access criteria hindered recovery for this vulnerable group.
Further research highlights inconsistencies in post-operative physiotherapy as well, with studies showing many patients do not routinely receive outpatient rehabilitative care after hip or knee replacements, illustrating a fragmented approach to follow-up treatment in high-volume NHS hospitals. In nursing homes, access to physiotherapy is even more limited, with studies revealing only a small minority of residents receive these essential services, often relying on privately employed therapists rather than NHS provision.
The broader pressure on NHS rehabilitation services, especially during and following the pandemic, has led to adaptive but imperfect solutions. For instance, pulmonary rehabilitation programmes shifted towards remote delivery during COVID-19, a strategy that brought benefits but also stark limitations due to patients’ varying technological access and needs. Equally, patients in rural and underserved communities face additional barriers including workforce shortages, poor digital infrastructure, and cultural factors, calling for decentralised and more locally accessible rehabilitation models.
Advocates warn that these accumulating pressures risk creating a postcode lottery in access to physiotherapy, with many, including those with muscle-wasting conditions, missing out on life-enhancing support. Muscular Dystrophy UK's chief executive, Andy Fletcher, described the situation as alarming and emblematic of wider NHS strains, emphasizing the critical need for equitable and consistent rehabilitation services.
In response, a Department of Health spokesperson reiterated the government’s recognition of physiotherapy’s vital role and its commitment to equipping NHS staff with the necessary facilities and resources. The spokesperson highlighted ongoing efforts to shift care from hospitals to community-centred neighbourhood health centres, aiming to deliver more convenient, coordinated rehabilitation closer to patients’ homes. However, experts and frontline staff stress that without addressing the immediate issues of space, equipment, and staffing, these ambitions may remain out of reach, and patients’ recoveries continue to suffer.
📌 Reference Map:
- Paragraph 1 – [1] (The Guardian)
- Paragraph 2 – [1] (The Guardian)
- Paragraph 3 – [1] (The Guardian)
- Paragraph 4 – [1] (The Guardian)
- Paragraph 5 – [1] (The Guardian), [2] (Evening Standard)
- Paragraph 6 – [1] (The Guardian), [3] (British Geriatrics Society)
- Paragraph 7 – [4] (PubMed), [5] (PubMed)
- Paragraph 8 – [6] (ACPRC), [7] (The Recovery Path)
- Paragraph 9 – [1] (The Guardian)
- Paragraph 10 – [1] (The Guardian)
Source: Noah Wire Services