According to the original report, artificial intelligence is reshaping medical diagnosis by analysing images, biomarkers and large clinical datasets to boost sensitivity, streamline workflows and provide clinicians with rapid, actionable insights that complement , rather than replace , human expertise. [1]
Clinical adoption in 2025 centres on a constellation of specialised tools: image‑first systems for mammography and retinal screening, real‑time CT/MRI triage engines, EHR‑integrated predictive models and portable point‑of‑care devices that bring interpretation to the bedside or community setting. These categories mirror the capabilities highlighted in the industry overview, which lists leading vendors and use cases now gaining traction in hospitals and clinics. [1]
Google Health’s mammography work exemplifies how imaging AI is being translated into practice. According to Google Health’s programme materials and clinical partnerships, models trained on tens of thousands of de‑identified mammograms have shown performance comparable with, and in some analyses superior to, individual radiologists, with lower false‑positive and false‑negative rates reported in U.K. and U.S. test sets. Google has moved from research to licensing and clinical studies in collaboration with partners to evaluate real‑world screening workflows. [2][4][3][5][7]
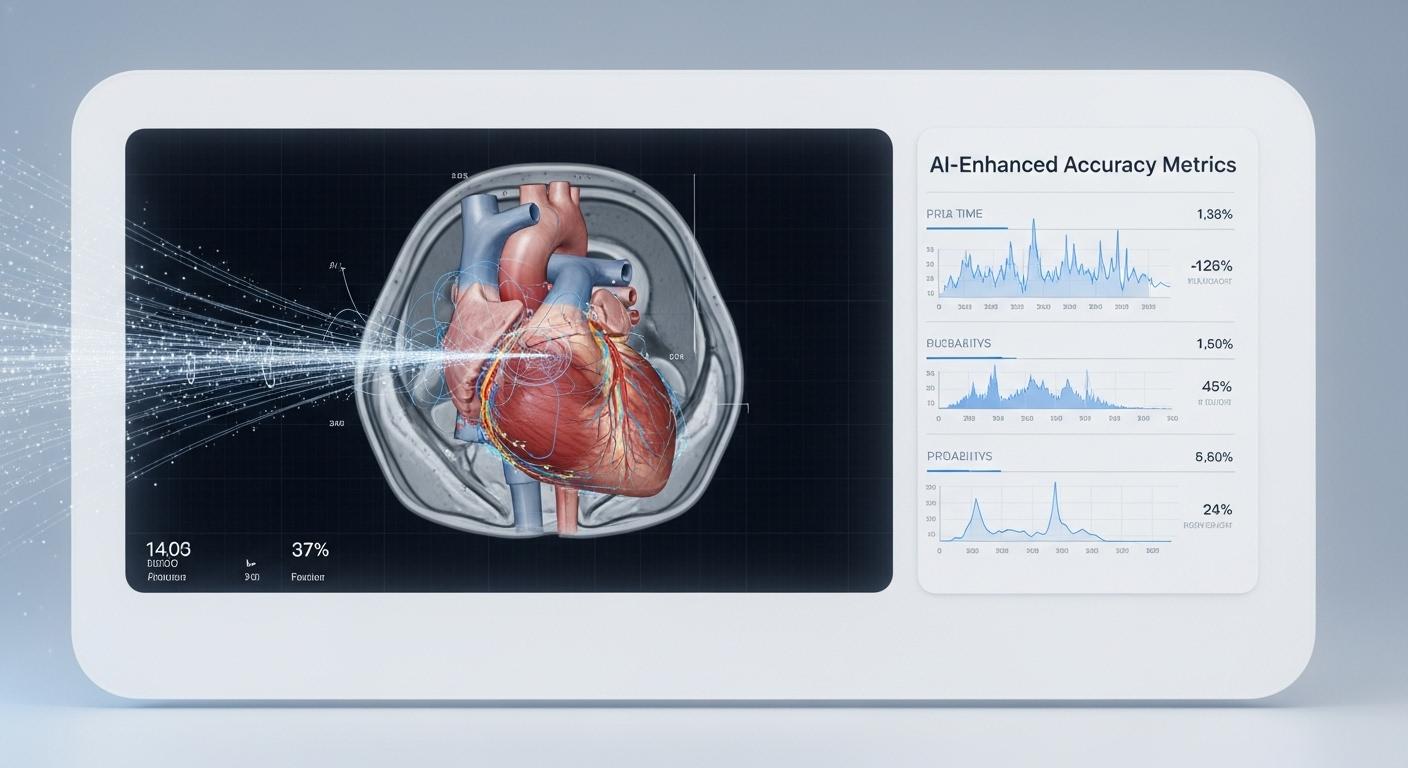
Other vendors cited in sector analyses provide complementary capabilities: real‑time stroke and haemorrhage flags for CT/MRI triage, AI guidance for echocardiography and handheld ultrasound, automated chest X‑ray screening for high‑volume settings, and pathology slide analysis using deep learning to improve grading consistency. Several commercial tools are already deployed across hundreds of hospitals, accelerating time‑to‑treatment in critical cases. [1]
Benchmarking studies and meta‑analyses cited in the reporting place diagnostic accuracy for imaging and clinical vignettes in the mid‑70s to low‑90s percent range, with AI often matching or exceeding average physician performance for specific tasks. Industry data also indicates that algorithms are increasingly used to support roughly two‑thirds of clinicians’ decision pathways, though the figures and clinical impact depend on the task, dataset and deployment context. [1][7]
Despite the gains, the sector faces persistent challenges: patient privacy and data governance, algorithmic bias arising from unrepresentative training sets, regulatory approval pathways that vary by jurisdiction, and the need for clinical workflows that preserve clear lines of responsibility and oversight. Ethical guidance and validation studies are being prioritised alongside technical development to ensure safety and equitable outcomes. [1]
Looking ahead, the most plausible near‑term trajectory is hybrid care models in which AI provides predictive analytics, triage and interpretation support while clinicians retain final judgement and patient stewardship. According to the reporting and programme partners, ongoing trials, broader regulatory review and tighter integration with EHRs will determine how rapidly AI becomes embedded in routine screening, triage and precision‑guided care. [1][2][4]
📌 Reference Map:
##Reference Map:
- [1] (TechTimes) - Paragraph 1, Paragraph 2, Paragraph 4, Paragraph 5, Paragraph 6, Paragraph 7
- [2] (Google Health) - Paragraph 3, Paragraph 7
- [3] (Google Blog: iCAD partnership) - Paragraph 3
- [4] (Google Blog: improving screening) - Paragraph 3, Paragraph 7
- [5] (Google Blog: Northwestern study) - Paragraph 3
- [6] (Google Health: ARDA/LYNA) - Paragraph 4
- [7] (VentureBeat) - Paragraph 3, Paragraph 5
Source: Noah Wire Services